The Way To Diagnose Severs Disease?
If your teen or preteen is complaining of heel pain, it might be Sever?s disease. No need to stress - this isn?t actually a ?disease,? but rather a common type of growing pain that only lasts a few weeks or months and doesn?t leave any long-term damage. Sever?s disease occurs in kids as they hit their adolescent growth spurt, usually between the ages of 8-13 for girls and 10-15 for boys. It?s most common among active kids that run, play basketball or soccer, or do gymnastics. Kids with flat feet, high arches, short leg syndrome, over-pronation (feet that roll inward when they walk) or who are overweight or obese also have an increased risk.
Causes
Predisposing Hereditary Factors: These are a biomechanical defect that one may be born with, which increases the chances of developing Sever's Disease. Short Achilles Tendon, When the Achilles Tendon is short from birth, it will exaggerate the tightness of this tendon that occurs during a child's growing years. This makes the pull of the Achilles Tendon on the heel's growth plate more forceful than normal, causing inflammation and pain, and eventually Sever's Disease. Short Leg Syndrome, When one leg is shorter than the other, the foot on the short leg must plantar flex (the foot and toes bend down) in order to reach the ground. In this way, the body tries to equalize the length of the legs. In order for the foot to plantar flex, the Achilles Tendon must pull on the heel with greater force than if the leg was a normal length. Thus the heel on the short leg will be more susceptible to Sever's Disease during the foot's growing years. Pronation. Is a biomechanical defect of the foot that involves a rolling outward of the foot at the ankle, so that when walking, the inner side of the heel and foot bears more of the body's weight than is normal (click here for more information about pronation). Pronation thus causes the heel to be tilted or twisted. In order for the Achilles Tendon to attach to the heel, it must twist to reach its normal attachment site. This will shorten or tighten the Achilles Tendon and increase the force of its pull on the heel's growth plate. This will increase the tightness of the Achilles Tendon during the foot's growing years, and may help to initiate bouts of Sever's Disease. Flat Arches and High Arches. Both of these biomechanical foot defects effect the pitch, or angle of the heel within the foot. When the heel is not positioned normally within the foot due to the height of the arch, the Achilles Tendon's attachment to the heel is affected. This may produce a shortening or tightening of the Achilles Tendon, which increases the force of its pull on the heel's growth plate. During the foot's growing years, abnormal arch height may contribute to the onset of Sever's Disease.
Symptoms
Symptoms include heel pain related to sports activities and worsen after those sport and exercise activities. However, some children who are not in a sport may also get this if they are physically active. If you notice that your child is ?walking on their toes? this is a sign of possible heel pain. The pain is usually on the back of the heel, the sides of the heel, the bottom of the heel, or a combination of all of these. We typically don't see swelling with this, however if pressure is applied to the sides of the heel pain may be reported. Sometimes the pain is so bad the child will have to limp, or take a break from sports activity either for a few days or few months.
Diagnosis
In Sever's disease, heel pain can be in one or both heels. It usually starts after a child begins a new sports season or a new sport. Your child may walk with a limp. The pain may increase when he or she runs or jumps. He or she may have a tendency to tiptoe. Your child's heel may hurt if you squeeze both sides toward the very back. This is called the squeeze test. Your doctor may also find that your child's heel tendons have become tight.
Non Surgical Treatment
Orthotics, The orthotics prescribed are made to align the foot in its correct foot posture. This will reduce stress and force at the site of the growth plate of the heel bone. Rest and Ice the heel 20 minutes before and after sporting activity. Calf muscle stretching exercises.
Recovery
This condition is self limiting, it will go away when the two parts of bony growth join together, this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join, usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
The Facts Not Fallacies About Achilles Tendon RuptureS
Overview
 An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).
An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears).
Causes
Causes of and contributors to Achilles tendon rupture include trauma (caused by injury, usually an acceleration injury such as pushing off or jumping up). Preceding tendon problems. Chronic Achilles tendonitis (can lead to small tears within the tendon, increasingly weakening it). Certain drug therapies/treatments. Drugs that have been linked to Achilles tendon rupture include. Fluoroquinolone antibiotics - after nearly 900 reports of tendon ruptures, tendonitis and other tendon disorders (most associated with the Achilles tendon) linked to Ciprofloxacin (Cipro) alone were collected in the U.S. Food and Drug Administration (FDA)?s database, at least one public-interest group petitioned the FDA to recommend that a "Black Box Warning" be added to Cipro's packaging. Some researchers speculate this class of antibiotics is toxic to tendon fibers, and that in some cases may reduce their blood supply. Patients should at least be more aware of the potential for ruptures so that they can be switched to other antibiotics at the onset of early warning signals such as tendon pain.
Symptoms
Patients present with acute posterior ankle/heel pain and may give a history of ?felt like someone kicked me from behind?. Patients may report a direct injury, or report the pain started with jumping or landing on a dorsiflexed foot. It is important to elicit in the history any recent steroid or flouroqunolone usage including local steroid injections, and also any history of endocrine disorders or systemic inflammatory conditions.
Diagnosis
When Achilles tendon injury is suspected, the entire lower lag is examined for swelling, bruising, and tenderness. If there is a full rupture, a gap in the tendon may be noted. Patients will not be able to stand on the toes if there is a complete Achilles tendon rupture. Several tests can be performed to look for Achilles tendon rupture. One of the most widely used tests is called the Thompson test. The patient is asked to lie down on the stomach and the examiner squeezes the calf area. In normal people, this leads to flexion of the foot. With Achilles tendon injury, this movement is not seen.
Non Surgical Treatment
Initial treatment for sprains and strains should occur as soon as possible. Remember RICE! Rest the injured part. Pain is the body's signal to not move an injury. Ice the injury. This will limit the swelling and help with the spasm. Compress the injured area. This again, limits the swelling. Be careful not to apply a wrap so tightly that it might act as a tourniquet and cut off the blood supply. Elevate the injured part. This lets gravity help reduce the swelling by allowing fluid and blood to drain downhill to the heart. Over-the-counter pain medication is an option. Acetaminophen (Tylenol) is helpful for pain, but ibuprofen (Motrin, Advil, Nuprin) might be better, because these medications relieve both pain and inflammation. Remember to follow the guidelines on the bottle for appropriate amounts of medicine, especially for children and teens. 
Surgical Treatment
Surgery may be indicated directly following injury rather than conservative care. Repair of an achilles tendon rupture is greatly varied for each clinical situation. There may be a direct repair of the ends of the tendon with suture, or possibly a tendon graft used to augment the tendon. Post-operatively, the period of immobilization will depend on the size of the defect that was repaired and how it was completed. Usually the immobilization is between 6-10 weeks. This repair may allow for a complete return to normal function, but in many instances the healing is complicated with adhesions and a partial loss of range of motion. There may be a continued soft tissue defect noted and a permanent or prolonged swelling.
Prevention
Good flexibility of the calf muscles plays an essential role in the prevention of Achilles tendon injuries. It is also important to include balance and stability work as part of the training programme. This should include work for the deep-seated abdominal muscles and for the muscles that control the hip. This might at first appear odd, given the fact that the Achilles are a good distance from these areas, but developing strength and control in this area (core stability) can boost control at the knee and ankle joints. Training errors should be avoided. The volume, intensity and frequency of training should be monitored carefully, and gradually progressed, particularly when introducing new modes of training to the programme. Abrupt changes in training load are the primary cause of Achilles tendinopathy.
Leg Length Discrepancy Shoes
Surgeries to lengthen a leg are generally only performed when there is a difference in leg length of greater than four centimeters. These types of surgeries can be more difficult and have more complications, such as infections, delayed healing, dislocations, and high blood pressure. In a several step process, bone lengthening surgeries involve cutting a bone in two in order to allow new bone growth to occur. After the bone is cut, a special apparatus is worn with pins that will pull the bone apart at approximately one millimeter per day. This causes osteogenesis, or new bone growth, in between the cut bone segments. A cast or brace may be required for several months after surgery to allow the new bone growth to harden and provide extra support.
Causes
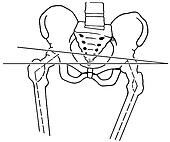
Leg length discrepancies can be caused by poor alignment of the pelvis or simply because one leg is structurally longer than the other. Regardless of the reason, your body wants to be symmetrical and will do its best to compensate for the length difference. The greater the leg length difference, the earlier the symptoms will present themselves to the patient. Specific diagnoses that coincide with leg length discrepancy include: scoliosis, lumbar herniated discs, sacroiliitis, pelvic obiliquity, greater trochanteric bursitis, hip arthritis, piriformis syndrome, patellofemoral syndrome and foot pronation. Other potential causes could be due to an injury (such as a fracture), bone disease, bone tumors, congenital problems (present at birth) or from a neuromuscular problem.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
Heel lifts and sole lifts are simple ways Pedorthists can compensate for leg length deficiencies. These small modifications can make a tremendous difference to a person?s comfort, balance and mobility. Although people do not always know if they have LLD if you have any of the symptoms I have mentioned you should consult a Pedorthist as treating your condition early will reduce the development of serious problems later on.

Surgical Treatment
Surgical options in leg length discrepancy treatment include procedures to lengthen the shorter leg, or shorten the longer leg. Your child's physician will choose the safest and most effective method based on the aforementioned factors. No matter the surgical procedure performed, physical therapy will be required after surgery in order to stretch muscles and help support the flexibility of the surrounding joints. Surgical shortening is safer than surgical lengthening and has fewer complications. Surgical procedures to shorten one leg include removing part of a bone, called a bone resection. They can also include epiphysiodesis or epiphyseal stapling, where the growth plate in a bone is tethered or stapled. This slows the rate of growth in the surgical leg.
Will Adult Aquired FlatFoot Need To Have Surgery ?
Overview
Posterior tibial tendon dysfunction is one of several terms to describe a painful, progressive flatfoot deformity in adults. Other terms include posterior tibial tendon insufficiency and adult acquired flatfoot. The term adult acquired flatfoot is more appropriate because it allows a broader recognition of causative factors, not only limited to the posterior tibial tendon, an event where the posterior tibial tendon looses strength and function. The adult acquired flatfoot is a progressive, symptomatic (painful) deformity resulting from gradual stretch (attenuation) of the tibialis posterior tendon as well as the ligaments that support the arch of the foot. 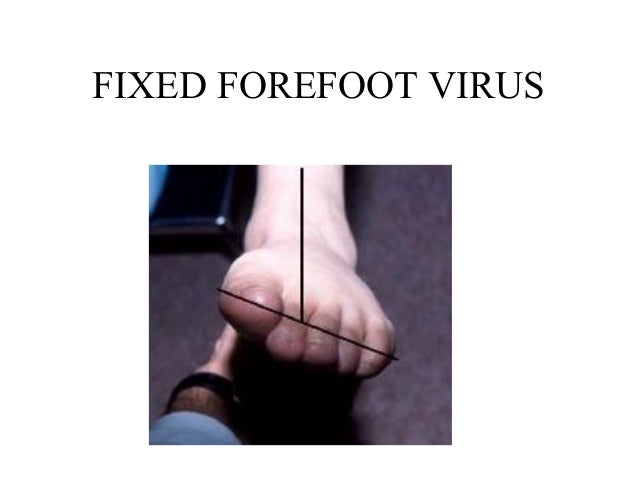
Causes
Obesity - Overtime if your body is carrying those extra pounds, you can potentially injure your feet. The extra weight puts pressure on the ligaments that support your feet. Also being over weight can lead to type two diabetes which also can attribute to AAFD. Diabetes - Diabetes can also play a role in Adult Acquired Flatfoot Deformity. Diabetes can cause damage to ligaments, which support your feet and other bones in your body. In addition to damaged ligaments, uncontrolled diabetes can lead to ulcers on your feet. When the arches fall in the feet, the front of the foot is wider, and outer aspects of the foot can start to rub in your shoe wear. Patients with uncontrolled diabetes may not notice or have symptoms of pain due to nerve damage. Diabetic patient don?t see they have a problem, and other complications occur in the feet such as ulcers and wounds. Hypertension - High blood pressure cause arteries narrow overtime, which could decrease blood flow to ligaments. The blood flow to the ligaments is what keeps the foot arches healthy, and supportive. Arthritis - Arthritis can form in an old injury overtime this can lead to flatfeet as well. Arthritis is painful as well which contributes to the increased pain of AAFD. Injury - Injuries are a common reason as well for AAFD. Stress from impact sports. Ligament damage from injury can cause the bones of the foot to fallout of ailment. Overtime the ligaments will tear and result in complete flattening of feet.
Symptoms
Patients often experience pain and/or deformity at the ankle or hindfoot. When the posterior tibial tendon does not work properly, a number of changes can occur to the foot and ankle. In the earlier stages, symptoms often include pain and tenderness along the posterior tibial tendon behind the inside of the ankle. As the tendon progressively fails, deformity of the foot and ankle may occur. This deformity can include progressive flattening of the arch, shifting of the heel so that it no longer is aligned underneath the rest of the leg, rotation and deformity of the forefoot, tightening of the heel cord, development of arthritis, and deformity of the ankle joint. At certain stages of this disorder, pain may shift from the inside to the outside aspect of the ankle as the heel shifts outward and structures are pinched laterally.
Diagnosis
Looking at the patient when they stand will usually demonstrate a flatfoot deformity (marked flattening of the medial longitudinal arch). The front part of the foot (forefoot) is often splayed out to the side. This leads to the presence of a ?too many toes? sign. This sign is present when the toes can be seen from directly behind the patient. The gait is often somewhat flatfooted as the patient has the dysfunctional posterior tibial tendon can no longer stabilize the arch of the foot. The physician?s touch will often demonstrate tenderness and sometimes swelling over the inside of the ankle just below the bony prominence (the medial malleolus). There may also be pain in the outside aspect of the ankle. This pain originates from impingement or compression of two tendons between the outside ankle bone (fibula) and the heel bone (calcaneus) when the patient is standing.
Non surgical Treatment
Treatment of Adult Acquired Flatfoot Deformity depends on the stage of progression, as mentioned above paragraphs. Below we will outline a variety of different treatment options available. Orthotics or bracing. To give your foot the arch the support it needs, your podiatrist or foot specialist may provide you with over the counter brace or a custom orthotic device that fits your shoe. Casting. In some cases, a cast or boot is worn to stabilize the foot and to give the tendon time to heal. Physiotherapy. Ultrasound treatments and exercises may help rehab the tendon and muscles. Medications. Over-the-counter (NSAIDS) such as ibuprofen can help reduce pain, inflammation and swelling associated with AAFD. Shoe Gear. Your podiatrist may suggest changes with your shoes you are wearing and inserts you need in your shoe to help support your arch. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.